Our Science
Shattuck is developing potentially first-in-class antibodies engineered to target DR3, the receptor for TL1A. Our approach confers the unique benefit of receptor blockade, which we believe will deliver both monotherapy and combination therapy strategies that have the potential to bring a new level of efficacy to patients suffering from IBD and other inflammatory and immune-mediated diseases.

TL1A and DR3 As a Foundational Target Axis in Immuno-Inflammatory Diseases
TL1A is a name of a protein our bodies produce that can cause inflammation through binding to a receptor known as DR3. TL1A and DR3 are members of a broad family of proteins, called the TNF superfamily, that are related to TNFɑ (the target of drugs like Humira® and Enbrel®). Pre-clinical studies have shown that when TL1A binds to DR3, inflammation becomes more severe in a variety of autoimmune conditions including inflammatory bowel disease, asthma, and arthritis. Accordingly, pre-clinical studies have demonstrated that blocking the interaction between TL1A and DR3 can reduce or resolve inflammation in these autoimmune conditions.
Several recent placebo-controlled Phase 2 clinical trials have shown that antibodies which bind to TL1A and block the interaction between TL1A and DR3 lead to high rates of clinical remission in patients suffering from either ulcerative colitis or Crohn’s disease. Each of these TL1A blocking antibodies (individually known as tulisokibart, afimkibart and duvakitug) have now begun Phase 3 clinical trials in both ulcerative colitis and Crohn’s disease.
Potential Advantages of Blocking DR3 Instead of TL1A
There are reasons to believe that blocking DR3 with SL-325 may be superior to blocking TL1A:

SL-325 may be less immunogenic than TL1A blocking antibodies
TL1A blocking antibodies bind to free TL1A in the serum. When TL1A antibodies are bound to circulating TL1A, this forms an immune complex. Immune complexes are a significant contributor to anti-drug antibody formation. Anti-drug antibodies present a significant challenge, and have led to treatment resistance and failure over time with similar medicines including Humira®, Simponi®, and Enbrel®. Immune complex formation is not expected with DR3 blocking antibodies because DR3 remains bound to the cell membrane. We believe that the potentially reduced immunogenicity profile of SL-325 may lead to greater efficacy and durability compared to TL1A blocking antibodies.

Due to the broad and stable expression of DR3, SL-325 may have superior efficacy than TL1A blocking antibodies
TL1A is selectively and transiently expressed within actively inflamed tissues, whereas DR3 is more abundant both at the site of inflammation and in nearby non-inflamed tissue. This may provide a means for SL-325 to provide more complete suppression of TL1A signaling, potentially preventing the spread of inflammation.

Targeting DR3 may enable development of bispecific antibodies, which has not been possible for TL1A directed antibodies
Two TL1A-directed bispecific antibodies (AMG966 and RG6730) caused anti-drug antibody formation in 100% of subjects following a single dose in Phase 1 clinical trials. Greater than 80% of those anti-drug antibodies were shown to neutralize target engagement. This unusually high degree of immunogenicity was attributed to large immune complex formation.
Because DR3 is a membrane-restricted target, immune complex formation is not expected for either monoclonal antibodies or bispecific antibodies targeting DR3, including SL-325 and our pipeline of bispecific antibodies.
SL-325
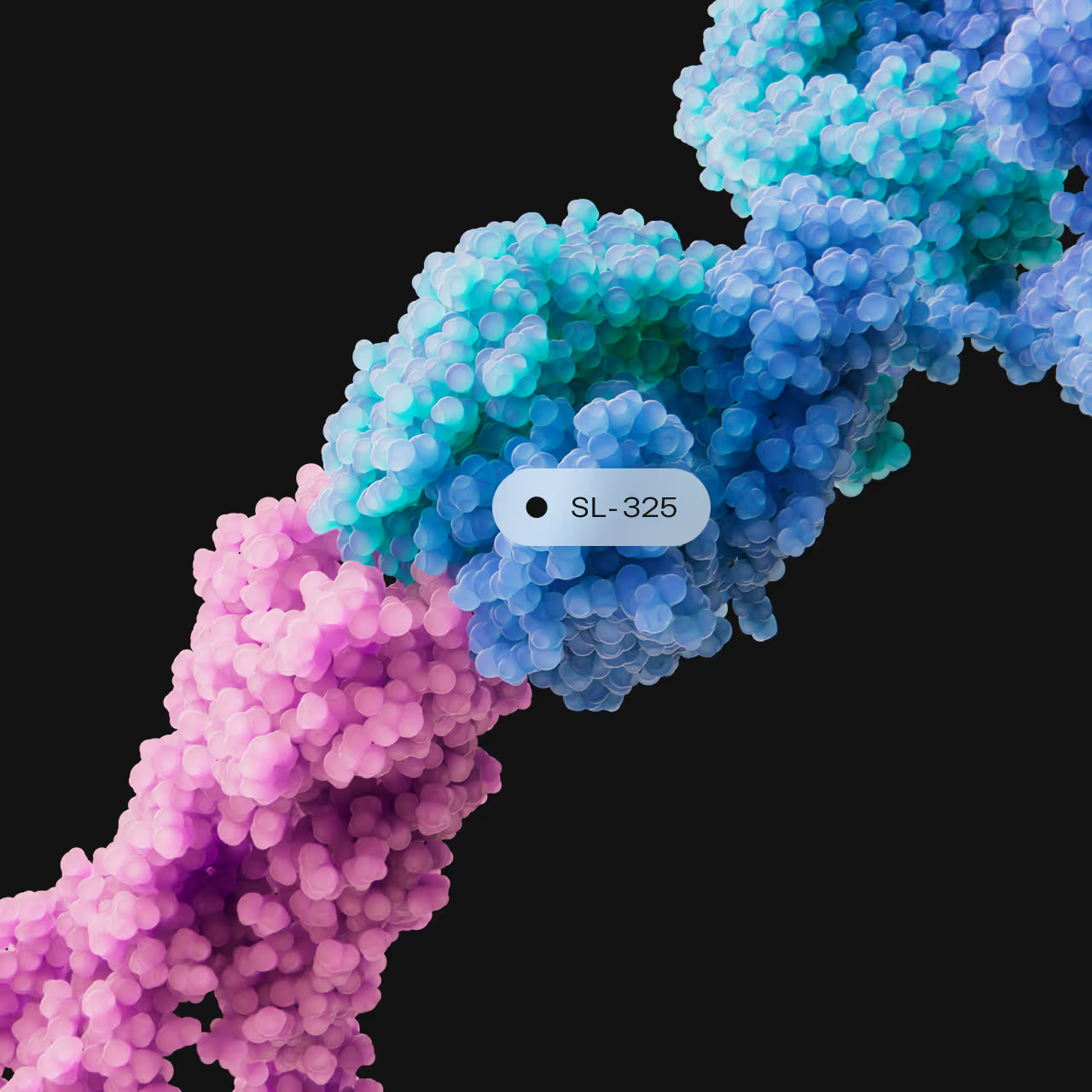
Antibodies which block TL1A signaling to DR3 have the potential to become the frontline standard of care in both ulcerative colitis and Crohn’s disease. A best-in-class antibody such as SL-325 could become a preferred therapy for many of the >3 million people suffering from inflammatory bowel disease worldwide, and become the backbone of future combination therapy strategies.
Because DR3 signaling sits upstream from a broad spectrum of inflammatory cytokines, the initial clinical activity observed in inflammatory bowel disease may have potential in other immuno-inflammatory diseases, including rheumatoid arthritis, psoriatic arthritis, atopic dermatitis, and hydradenitis suppurativa.
- Efficiently blocks soluble trimeric and membrane bound TL1A binding to DR3
- pM binding affinity to DR3
- Highly specific, and does not cross-bind to decoy receptor 3 (DcR3)
- Fully Fc-silenced to prevent unwanted immune activation
- Does not cause internalization of DR3, leading to durable receptor occupancy
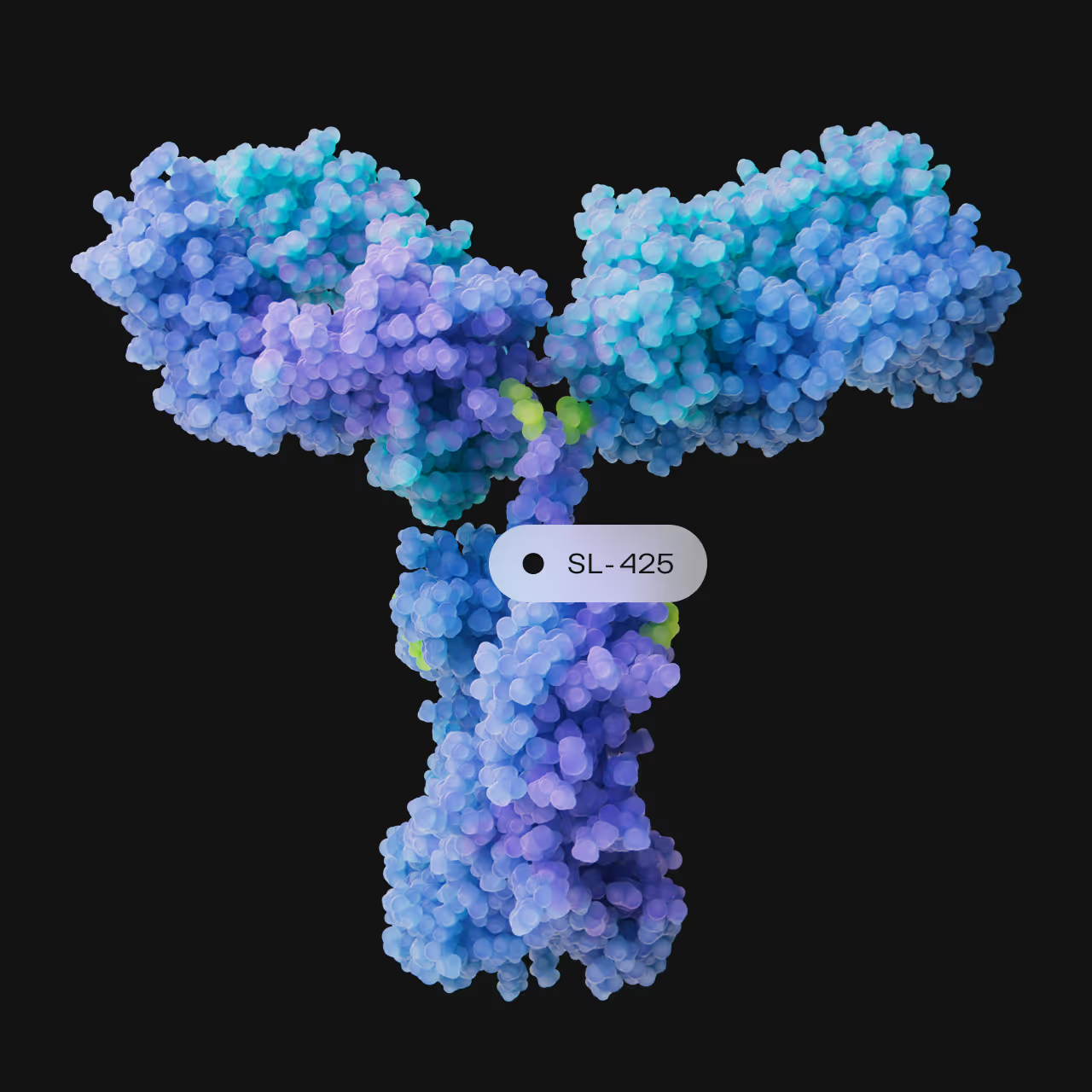
SL-425
SL-425 is a half-life extended version of SL-325. Shattuck may select to advance one or both of SL-325 and SL-425 in future studies, based on the pharmacokinetic and pharmacodynamic properties of each antibody. We expect that each antibody will have properties that could be differentially advantageous in distinct diseases, and will provide an opportunity to balance TL1A/DR3 biology with administration regimens that are convenient for patients.